Patrick D. McGorry et. al, a group of psychiatrists in Australia, conducted the NEURAPRO trial to determine omega-3’s effect on patients who are high-risk and may develop psychosis. They argue that omega-3 does not affect the risk of developing schizophrenia or its symptoms.
Effect of ω-3 Polyunsaturated Fatty Acids in Young People at Ultrahigh Risk for Psychotic Disorders: The NEURAPRO Randomized Clinical Trial
By: Patrick D McGorry, Barnaby Nelson, Connie Markulev, Hok Pan Yuen, Miriam R Schäfer, Nilufar Mossaheb, Monika Schlögelhofer, Stephan Smesny, Ian B Hickie, Gregor Emanuel Berger, Eric Y H Chen, Lieuwe de Haan, Dorien H Nieman, Merete Nordentoft, Anita Riecher-Rössler, Swapna Verma, Andrew Thompson, Alison Ruth Yung, G Paul Amminger
Jan. 1, 2017
Abstract
Importance: A promising treatment to prevent onset and improve outcomes in patients at ultrahigh risk for psychosis is dietary supplementation with long-chain ω-3 polyunsaturated fatty acids (PUFAs).
Objective: To determine whether treatment with ω-3 PUFAs in combination with a high-quality psychosocial intervention (cognitive behavioral case management [CBCM]) is more effective than placebo plus CBCM.
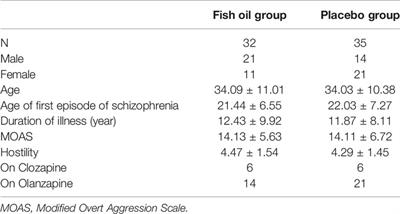
Design, setting, and participants: NEURAPRO, a double-blind, placebo-controlled, randomized clinical trial, was conducted from March 1, 2010, to September 30, 2014, in 10 specialized early psychosis treatment services in Australia, Asia, and Europe. The primary analysis used the intention-to-treat approach.
Interventions: A daily dose of 1.4 g of ω-3 PUFAs or placebo (paraffin oil), plus 20 or fewer sessions of CBCM over the 6-month study period.
Main outcomes and measures: The primary outcome was transition to psychosis status at 6 months. The secondary outcomes were general levels of psychopathology and functioning, as assessed by the Brief Psychiatric Rating Scale (BPRS) (range, 24-168), Scale for the Assessment of Negative Symptoms (SANS) (range, 0-125), Montgomery-Åsberg Depression Rating Scale (MADRS) (range, 0-60), Young Mania Rating Scale (YMRS) (range, 0-44), Social and Occupational Functioning Assessment Scale (SOFAS) (range, 0-100), and the Global Functioning: Social and Role scale (range, 0-10). For SOFAS and Global Functioning: Social and Role scale, higher scores were better; for other measures, lower scores were better.
Results: In this study of 304 adults at ultrahigh risk for psychotic disorders, 153 (50.3%) received ω-3 PUFAs and 151 (49.7%) received placebo. In all, 139 (45.7%) were male; mean (SD) age was 19.1 (4.6) years. The Kaplan-Meier-estimated 6-month transition rates were 5.1% (95% CI, 1.3%-8.7%) in the control group and 6.7% (95% CI, 2.3%-10.8%) in the ω-3 PUFA group. At 12 months, the rates were 11.2% (95% CI, 5.5%-16.7%) in the control group and 11.5% (95% CI, 5.8%-16.9%) in the ω-3 PUFA group. No significant difference was observed between the transition rates of both groups (hazard ratio, 1.1; 95% CI, 0.55-2.23; P = .76, stratified log-rank test).
Conclusions and relevance: This trial clearly failed to replicate the findings of the original single-center trial. The most likely explanation is that ω-3 PUFAs lack efficacy under these conditions. However, the lower-than-expected transition rate may have prevented a test of the main hypothesis. Given the substantial symptomatic and functional improvement in both groups, the other treatments received (ie, CBCM and antidepressants) likely produced a ceiling effect beyond which ω-3 PUFAs, even if effective, could not be shown to confer additional benefits. Nevertheless, the main conclusion is that ω-3 PUFAs are not effective under conditions where good quality, evidence-based psychosocial treatment is available.