January 2019
Ann Williamson
Hypnosis can be seen as ‘a waking state of awareness, (or consciousness), in which a person’s attention is detached from his or her immediate environment and is absorbed by inner experiences such as feelings, cognition and imagery’.1 Hypnotic induction involves focusing of attention and imaginative involvement to the point where what is being imagined feels real. By the use and acceptance of suggestions, the clinician and patient construct a hypnotic reality.
Everyday ‘trance’ states are part of our common human experience, such as getting lost in a good book, driving down a familiar stretch of road with no conscious recollection, when in prayer or meditation, or when undertaking a monotonous or a creative activity. Our conscious awareness of our surroundings versus an inner awareness is on a continuum, so that, when in these states, one’s focus is predominantly internal, but one does not necessarily lose all outer awareness.
Hypnosis could be seen as a meditative state, which one can learn to access consciously and deliberately, for a therapeutic purpose. Suggestions are then given either verbally or using imagery, directed at the desired outcome. This might be to allay anxiety by accessing calmness and relaxation, help manage side effects of medications, or help ease pain or other symptoms. Depending on the suggestions given, hypnosis is usually a relaxing experience, which can be very useful with a patient who is tense or anxious. However, the main usefulness of the hypnotic state is the increased effectiveness of suggestion and access to mind/body links or unconscious processing. Hypnosis can not only be used to reduce emotional distress but also may have a direct effect on the patient’s experience of pain.2
Hypnosis in itself is not a therapy, but it can be a tool that facilitates the delivery of therapy in the same way as a syringe delivers drugs. Hypnosis does not make the impossible possible, but can help patients believe and experience what might be possible for them to achieve.
Hypnotic states have been used for healing since humankind has existed, but because hypnosis can be misused for so-called entertainment and has been portrayed in the media as something mysterious and magical, supposedly out of the hypnotic subject’s control, it has been viewed with distrust and scepticism by many health professionals. However, recent advances in neuroscience have enabled us to begin to understand what might be happening when someone enters a hypnotic state,3–8 and evidence is building for the use of hypnosis as a useful tool to help patients and health professionals manage a variety of conditions, especially anxiety and pain.
Landry and colleagues9 and Jensen and Patterson10 give good and comprehensive information on recent research into the neural correlates of hypnosis. The study of hypnosis is complex and many factors such as context, expectation and personality affect hypnotic response as well as the suggestions used.
As clinicians, we know that simply knowing something cognitively does not necessarily translate into being able to control emotions such as fear and anxiety. A simple ‘model’ that can be used to help patients understand that this is quite a usual response is that of right/left brain, which can also correlate with conscious/unconscious and intellectual/emotional processing.
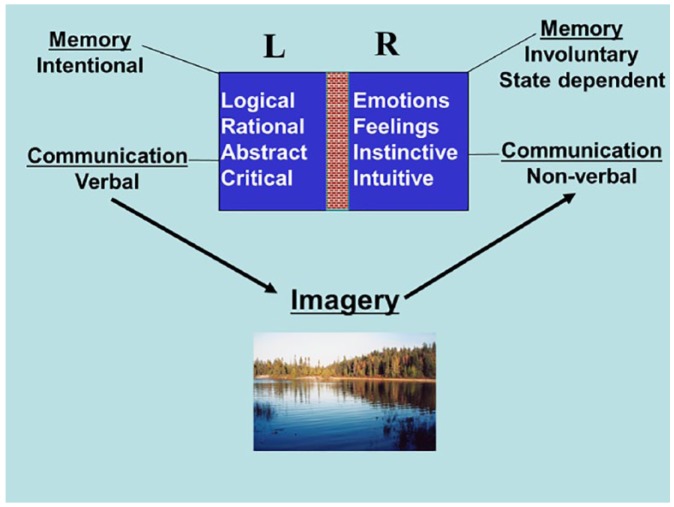
From the diagram, it can be seen that to communicate effectively to both types of our processing, we need more than words; we need to use words that evoke imagery. It is no surprise, therefore, that all the greatest teachers use metaphor, parable and story to convey their teachings.
The brain has two cerebral hemispheres, and while in our normal waking state, the left brain tends to be more dominant and could be likened to our ‘conscious mind’. This communicates verbally and is the more intellectual, conscious and rational part of ourselves. When we relax or become deeply involved in some activity, our right brain becomes more dominant. The right brain could be seen to be the more emotional, creative part of ourselves that communicates with symbols and images, and could be seen as our ‘unconscious mind’. There is always a difficulty in telling ourselves not to be upset or anxious because words are not the language of the right brain. But one can paint a word picture using guided imagery or metaphor.
While this description may oversimplify the neural processing of the left and right hemispheres, it is a useful way to explain hypnosis to patients.
Neuroimaging research has demonstrated that subjective changes in response to suggestion are associated with corresponding changes in brain regions related to the specific psychological function in question.11,12 When someone imagines something in hypnosis (colour, sound, physical activity and pain), recent neuroscience findings show us that similar areas of the brain are activated as when the person has that experience in reality. Derbyshire and colleagues13 showed that both physically induced and hypnotically induced pain are accompanied by activations in areas associated with the classic ‘pain matrix’. Similar findings have been shown with visual and auditory suggestions.14,15
When patients are highly anxious, they are operating at an emotional, rather than cognitive level, and one can engage and direct their creative imagination towards what is useful for them. Anxious patients are using their imagination to create possible catastrophic scenarios, which generates even more anxiety and hence more adrenaline, which can then spiral into panic.
Patients may feel that they are being overwhelmed by their emotions, but if the health professionals can engage their attention, direct their imagination to feeling calm or to re-experience some positive past experience or activity and give positive suggestions, then the patients will start to feel calmer and more able to cope.
To enter hypnosis, one needs to focus attention (this is done during a hypnotic induction), and there are many ways to achieve this. A candle flame or a computer screen could be a visual focus. An auditory focus could be music, chanting or using mantras. Induction could be mainly kinaesthetic, such as in progressive muscular relaxation (PMR) or could use ‘involuntary’ (or ideomotor) movement. One of the simplest methods is to engage the patient’s imagination using revivification (or re-experiencing) of an experience, a daydream or fantasy. Hypnosis can be used formally in a therapeutic session or informally in conversation by directing the patient’s focus and engaging their imagination.
Patients can then be taught self-hypnosis, which means they can enter this state deliberately at will, to utilise imagery and suggestion to help themselves.16 In the clinical setting, the health professional wants to avoid dependence and save time and money, and studies have shown that hypnotic interventions can be very cost-effective.17 Montgomery and colleagues18 randomised control trial of 200 breast cancer patients using a 15-min session of hypnosis or structured attention to control side effects after surgery also showed reduced medical costs with the hypnosis intervention.
There is a strong case for more research in the field of hypnosis in palliative care, where mind-body interventions are increasingly accepted as part of comprehensive excellent cancer care (even in large cancer centres that once focused only on drug trials).
Hypnosis research takes place in laboratory conditions and usually compares results between ‘highs’ and ‘lows’; in other words, those who are highly hypnotisable and those who are not. It has been shown that hypnotisability is a genetic trait and follows a Gaussian or bell-shaped distribution, so most research into hypnotic responding focuses on 10% of the population. In the clinical context, we have to work with everyone, and even if hypnosis is not used in a formal way, it can inform one’s approach to the patient and the language used. For experimental purposes, the procedure must be standardised and all variables controlled as much as possible. In the clinical context, hypnosis is tailored to the individual patient and their responses, and the motivation is very different from the laboratory situation.
Although there is increasing evidence for the usefulness and cost-effectiveness of using hypnosis in a wide variety of conditions, it is difficult to get funding for hypnosis because of a shortage of randomised control trial support (the gold standard so beloved of Trusts, CCGs, research funders and all clinical trialists). In a Catch-22 situation, one of the major difficulties in undertaking any hypnosis research in the United Kingdom is lack of funding. One major factor in this is the World Health Organization classification of hypnosis as a ‘Complementary Therapy’. This puts hypnosis in the same category as various other approaches of dubious scientific credibility and effectively bars researchers into hypnosis obtaining funding. Also, much hypnosis is done by individual clinicians in a private practice, a community setting or as an individual in a department.











