2021
Abhijit Nair, Praveen Sharma, and Manish Kumar Tiwary
To the Editor,
The severity of respiratory illness in COVID-19 depends on the imbalance between the pro-inflammatory and anti-inflammatory mediators in the lung parenchyma. The phases of the illness have been divided into the early respiratory tract infection followed by acute inflammation. The third phase is variable depending on patient characteristics i.e. presence of co-morbidities, viral load exposed, baseline immunity, the initiation of early treatment. There could be either resolution of the illness or severe illness.
Severe illness leads to cytokine storm (IL-6, TNF-α), leaky capillaries, hypoxic respiratory failure, multiorgan involvement leading to adult respiratory distress syndrome (ARDS) and subsequently invasive or non-invasive ventilation, shock all of which contributes to significant morbidity, and subsequent mortality.
The severe illness also leads to a hypercoagulable state which is evaluated using d-dimer and fibrin degradation products and managed with heparin (unfractionated or low molecular weight). TNF-α released during cytokine storm causes endothelial damage which leads to thrombosis. The thromboembolic events occurring thereafter contribute to significant morbidity and mortality.
Cytokines like IL-6, TNF-α eventually leads to the release of reactive oxygen species (ROS) and reactive nitrogen species from the mitochondria which is responsible for end-organ damage, thrombosis, and shock [Figure 1].
Presence of comorbidities like hypertension, diabetes mellitus, ischemic heart disease, respiratory ailments, chronic kidney disease, obesity and the elderly age groups are the ones with a low baseline immunity and thus are easily susceptible to develop serious illness once COVID-19 positive.
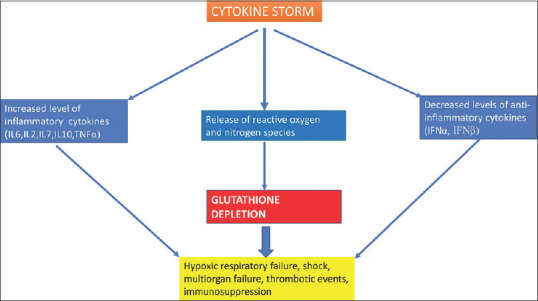
Figure 1
Image showing the cascade following cytokine storm in COVID-19 disease
The human body is naturally equipped with enzymatic and non-enzymatic antioxidant systems to prevent damage to cells, and vital organs due to free radicals. Glutathione peroxidase, catalase and superoxide dismutase are the enzymatic antioxidants. The non-enzymatic antioxidants are vitamin E, vitamin C, thiol antioxidants (Glutathione, Thioredoxin and lipoic acid), melatonin, carotenoids, and natural flavonoids.[2] In vivo, scavenging of ROS is predominantly mediated by Glutathione and glutathione peroxidase which is its regulator enzyme.
When production of ROS is uncontrolled there is depletion of glutathione as a result of which the patient gets susceptible to immunosuppression, organ damage, increased vascular permeability, shock, and thrombotic events. N-acetyl-cysteine is a by-product of glutathione and on supplementation increases levels of glutathione in the tissues by providing the amino acid cysteine. Normal intracellular glutathione is necessary for preserving immunity (lymphocytes and macrophages), optimal T-lymphocyte function and proliferation, and also in preventing apoptosis.[3] Glutathione deficiency also leads to reduced formation of anti-inflammatory cytokines like IFN-α and IFN-β.[4] Studies in viral illness have demonstrated antiviral, antioxidant, anti-inflammatory, and immunity enhancing properties of glutathione.
Polonikov observed in 4 diabetic patients recruited in genetics study of redox homeostasis that blood levels of Glutathione were low and that of ROS were high in moderate to severe COVID-19 disease than in patients who had mild disease.[5] The author also hypothesized that patients in whom Glutathione deficiency is expected i.e. elderly patients, patients with comorbidities, smokers and patients who have deficiency due to reduced intake of fresh fruits and vegetables are the one who might have a serious course of illness. Therefore, the hypothesis that replenishing Glutathione levels by exogenous administration intravenously could prevent serious COVID19 related illness needs to be explored with well-designed studies.
In a review by Khanfar et al.,[6] the authors described the pathophysiology of the failure of immune system, organ damage due to oxidative stress in presence of glutathione deficiency in the tissues. Authors suggested that Glutathione deficiency has a crucial role in having poor outcomes in patients with covid19 disease and therefore mandates supplementation of glutathione is susceptible patients. Guloyan et al.[7] recommended the use of liposomal glutathione in COVID-19 illness and hypothesize the benefits could be similar to that seen when used in tuberculosis, and HIV patients i.e. by reducing oxidative stress, inflammation, and by enhancing immunity when used in a dose ranging from 500 mg to 2 gm per day. At present, there is no consensus regarding the dose of liposomal Glutathione required to confer anti-inflammatory, antioxidant, and immune enhancing properties in patients with COVID-19 illness.
To conclude, Glutathione supplementation appears safe and could possibly be helpful in certain groups of patients when used along with other modalities of treatment of COVID-19 disease in early stages before organ damage has set in. Estimating Glutathione is not done routinely therefore clinicians should identify patients at risk of Glutathione deficiency based on history and other details. At present, the data supporting Glutathione supplementation appears anecdotal. Well-designed studies could enlighten the clinicians regarding efficacy of supplementation of glutathione and the dose required during early stages of COVID-19 disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.










