By: Raphael Underwood
Feb. 15, 2017
Psychotic illnesses, such as schizophrenia, develop gradually, beginning with subtle changes in perceptual experiences and thought processes. These changes evolve into a ‘prodromal’ phase characterised by subthreshold positive symptoms such as infrequent/less intense hallucinations and delusions (Yung, McGorry, et al., 2004). Individuals in the prodromal phase are termed Ultra-High Risk (UHR) (Yung & McGorry, 1996).
Observational studies have identified conversion rates from UHR to psychosis of:
- 17.7% at 6 months,
- 21.7% at 12 months,
- and up to 31.5% over 3 years (Fusar-Poli et al., 2012).
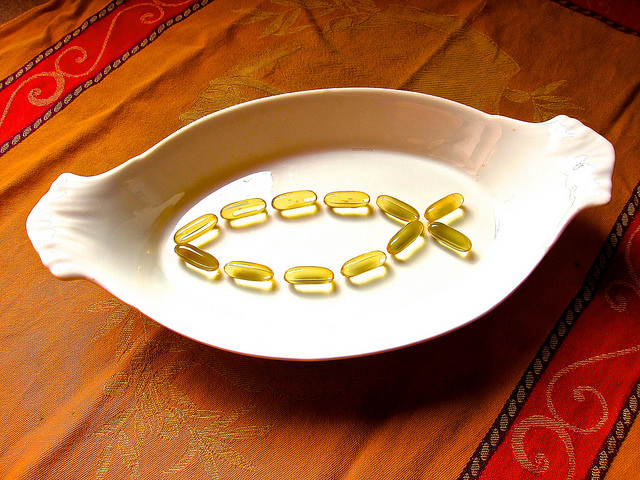
Much research has been dedicated towards preventing the transition from UHR status to psychotic illness (Yung, Phillips, et al., 2004). Eleven trials have assessed the effectiveness of talking therapies and pharmacological interventions, alone or combined, in UHR groups (van der Gaag et al., 2013). From these trials, cognitive behavioural therapy (CBT) and long-chain Omega-3 fatty acids (PUFAs) emerged as effective first-line treatments.
PUFAs were found to be effective not only during the period of treatment (Amminger et al., 2010), but also up to 7 years later (Amminger et al., 2015). These are exciting findings as conventional antipsychotics carry undesirable side-effects and an increased risk of adverse events (Kane & Correll, 2017). In a newly published study (McGorry et al., 2017), the authors attempted to replicate these impressive findings.