This research shows how alkalizing the blood pH was efficient in curing osteo –arthritis (OA). Accordingly, patients had significant decrease in pain, tenderness and stiffness of the hand joints.
Non-allopathic adjuvant management of osteoarthritis by alkalinisation of the diet
David P. van Velden,corresponding author | Helmuth Reuter | Martin Kidd | and F. Otto Müller
Published online 2015 Apr 21
Abstract
Background
Osteoarthritis (OA) is a chronic condition. Nonsteroidal anti-inflammatory drugs recommended for treatment have serious adverse effects. A compelling body of anecdotal evidence alerted the authors to the therapeutic potential of dietary supplementation with Multiforce® (MF) Alkaline Powder for relief of OA symptoms.
Aim
The aim of the study was to test the hypothesis that dietary supplementation with MF relieves clinical signs and symptoms of OA of the hands.
Setting
The study was done at the MEDSAC hospital in Somerset West, Western Cape, South Africa.
Methods
The research was conducted in two stages. An open interventional study (n = 40) confirmed the notion that MF 7.5 g twice daily is likely to be an effective alternative or adjunct for relief of symptoms of OA of the hands. The main study was conducted with 100 eligible, consenting volunteers (aged 47–89 years) according to a randomised, placebo-controlled, crossover design. Study duration was 56 days, 28 days per regimen; crossover to alternate regimens took place on day 28.
Results
Compared to placebo, MF intake over 28 days was associated with significant reductions (p < 0.005) in pain, tenderness and stiffness of interphalangeal and metacarpophalangeal joints of the hand. Confirmation of systemic alkalinisation by MF, which is rich in organic anions in the form of citrate salts, was reflected by a significant and sustained increase in urine pH.
Conclusion
A dietary supplement, Multiforce® Alkaline Powder, containing citrate salts which are converted into bicarbonate in vivo, was efficacious and safe as sole therapeutic intervention, significantly attenuating OA-associated signs and symptoms of the hands.
Introduction
Osteo-arthritis (OA) is a major cause of morbidity, affecting 60% of men and 70% of women over the age of 65 years.1 Current therapeutic approaches, including allopathic (Western) medicine, fail to prevent initiation and progression of OA, and some have life-threatening side-effects. The rapidly rising rates of complex, chronic disease are creating an unsustainable burden on the national economy in both direct (e.g. treatment) and indirect (e.g. lost productivity) costs.
These chronic and degenerative diseases cannot be effectively treated with drugs alone. As a matter of fact, chronic drug use for these conditions is not only costly but often has serious side-effects. Popular analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) such as celecoxib, diclofenac, ibobrufen, naproxen and aspirin have confirmed risk for heart disease and internal bleeding.2,3 Paracetamol can damage the liver. Allopathic medicines often do not cure these diseases, but rather mask the symptoms.
The incidence of OA increases with age, and ageing patients present with comorbidities that add to the complexity of treatment. Degeneration of joint cartilage is still the most important pathophysiological feature of OA. Tissues surrounding the joints, such as muscles, bones, tendons and ligaments, are also involved in the disease process. Recommendations for management of OA comprise non-pharmacological and pharmacological approaches. Non-pharmacological interventions include education and self-management, referral to a physical therapist, aerobic muscle-strengthening and water-based exercises, weight reduction, diet interventions, walking aids, knee braces, therapeutic footwear and insoles, thermal modalities, transcutaneous electrical nerve stimulation and acupuncture. Pharmacological treatments consist of paracetamol, systemic and topical cyclo-oxygenase-2 (COX-2) non-selective and selective inhibitors, classified as NSAIDs, topical capsaicin, intra-articular corticosteroids and hyaluronates, glucosamine and/or chondroitin sulphate and diacerin for possible structure-modifying effects, and use of opioid analgesics and tramadol for the treatment of refractory pain.4,5 Methotrexate, which has immunosuppressive and anti-inflammatory effects, is promising, but this drug may have serious side-effects, including liver disease, lung inflammation, increased susceptibility to infection, and suppression of blood cell production in the bone marrow. Studies with disease-modifying drugs in management of OA, such as bisphosphonates with the aim of inhibiting increased bone turnover, did not produce positive results.1
Long-term use of systemic NSAIDs to relieve OA symptoms could cause serious adverse events, such as gastro-intestinal bleeding, renal damage, and induction or aggravation of bronchial asthma and cardiovascular complications.2 The effect of COX-2 inhibitors on renal function is still tenuous. Of great concern has been the voluntary withdrawal of rofecoxib (Vioxx®) from the market in 2004 because of an increased risk of serious cardiovascular events, including heart attacks and stroke amongst patients taking Vioxx® compared to patients receiving placebo.6
Dietary considerations
The typical ‘Western diet’ is considered acidogenic due to the greater acid load contained in animal products, and is low in fruit and vegetables, resulting in a state of overlooked low-grade chronic, compensated metabolic acidosis.7 The ensuing acidotic stress and hypoxia may play a role in the pathophysiology of OA.8 In response to states of diet-derived metabolic acidosis, the kidney implements compensating mechanisms to restore the acid-base balance.
In South Africa there is compelling anecdotal evidence that an alkaline diet supplement, Multiforce® (MF) Alkaline Powder, has beneficial effects in patients with primary OA prompted this research to objectively explore the influence of dietary supplementation with MF on symptoms and signs of OA.
Aim
The aim of the study was to test, by means of a randomised controlled trial, the hypothesis that dietary supplementation with MF relieves clinical signs and symptoms of OA of the hands.
Research methods and design
The research comprised two stages, a pilot study and the main study.
In the pilot, a single-centre, open study of the efficacy and safety of MF in participants (n = 40) with OA revealed significant improvements (p < 0.005) in all parameters assessed. Side-effects were negligible (unpublished data).
The pilot study was followed by a single-centre, double-blind, placebo-controlled crossover study of the efficacy and safety of MF in participants with OA of the hands (n = 100), which is the subject of this article.
Both protocols were approved by the Ethics Committee for Human Research of Stellenbosch University (SU Ethics ref no: 10/02/009).
Study population
One hundred (100) consenting and responsible adult male and female volunteers (47–89 years of age; mean 65 years) with symptoms and signs of OA of the hands (left or right), with or without current allopathic treatment, fulfilling the inclusion criteria were recruited in Somerset West and surrounding areas.
For inclusion participants had to be able to understand and follow the instructions of the protocol; be mobile enough to attend visits to the clinic; give informed consent; be willing, committed, and able to return for all clinic visits and complete all study-related procedures; be able to engage in telephone communication; be compliant with the American Rheumatism Association classification of OA;9 and be able to complete a daily pain visual analogue scale (VAS) and the validated Stanford Health Assessment Questionnaire (HAQ) 20-item disability scale at each of the six visits. The two-page HAQ-DI (disability index)10 was used.
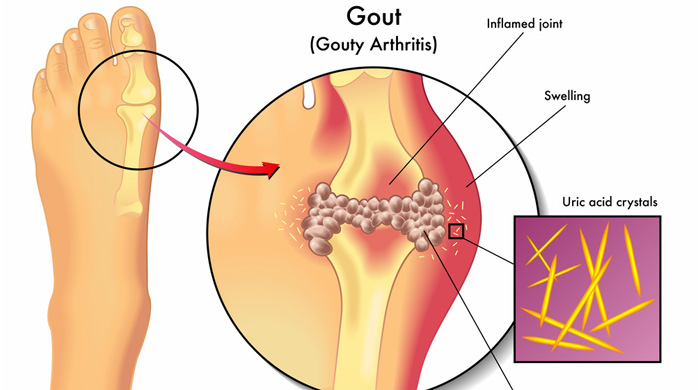
Exclusion criteria were, inter alia, gout or serum uric acid equal to or greater than 0.45 mmoL/L, rheumatoid arthritis or high-sensitivity C-reactive protein (hs-CRP) > 20 mg/dl, known or suspected current infection or recurrent infectious disease of a joint, immunosuppressive therapy, history of demyelinating disease or symptoms suggestive of multiple sclerosis, psoriasis, intra-articular, intramuscular or intravenous glucocorticoid therapy eight weeks prior to the screening visit, glomerular filtration rate of < 30 mL/min (as per the Modification of Diet in Renal Disease index), history of acute or recurrent urinary tract infections, ‘abnormal’ clinical chemistry and haematology values, such as serum transaminases and alkaline phosphatase > 2 x upper limit of normal, full blood count outside normal limits, and abnormal serum electrolyte levels.
In addition, patients with any other arthritic or medical condition that in the opinion of the investigator could compromise participation or interfere with evaluations were excluded, as were those with a history of drug abuse within the five years prior to the screening visit, a history of alcohol abuse or current intake of 21 or more alcohol-containing drinks per week, and any investigational drug taken within three months or five drug half-lives, whichever was the longer period, prior to screening.
Results
One hundred and fifty-nine patients were screened for OA of the hands, and 100 who fulfilled the inclusion criteria were enrolled in the study. They were randomly assigned into two groups, A and B (verum n = 50 group A, and placebo n = 50 group B, specifying which treatment came first). Drop-outs were not replaced. Two patients, one from each treatment group, dropped out because they relocated, and 98 patients completed the trial. Eighty-eight per cent of participants were female.
All participants had primary OA of the IP or MP joints of the hands.
Acceptability and tolerance of supplement
No serious adverse events occurred. Three patients reported mild diarrhoea whilst on the verum intervention. Overall acceptability was good.
Value of the Stanford HAQ
During the two-month intervention trial no significant changes were found in functional ability in dressing and grooming, arising, eating, walking, hygiene and reach. Most participants had only difficulty in grip strength (opening jars and taps) and in performing certain household activities and gardening. Although they did experience some improvement in the function of the hands on the verum, this was not statistically significant. It is clear that this questionnaire is more appropriate for patients with rheumatoid arthritis with severe functional disability, and it did not help in assessing the influence of the intervention on OA in those with longstanding OA and no other serious functional disabilities. Patients with OA of the hands have low functional disability not amenable to change.